Maternal cardiovascular compromise and fetal hypoxia are well recognized side effects of supine positioning in advanced pregnancy. Supine hypotensive syndrome (SHS) is a clinical diagnosis loosely defined as a clinically significant decrease in maternal cardiac output due to presumed compression of the inferior vena cava and aorta by the gravid uterus within a few minutes (3-10 minutes) of assuming the supine position [1]. SHS can be rapidly reversed with decompression of the great vessels.
What is "clinically significant?"
A critical threshold has not been established, but a drop in systolic blood pressure in the supine position (compared to lateral) of 15-30 mmHg or 20-30% from baseline is consistent with supine hypotensive syndrome.
Only 8-12% of third trimester parturients are thought to experience SHS [2]. In this subset of patients, the drop in cardiac output can present as a spectrum from transient asymptomatic hypotension to severe clinical symptoms. Characteristic symptoms include dizziness, nausea, vomiting, abdominal or chest discomfort and restlessness. Maternal hypotension can decrease uteroplacental perfusion and cause fetal hypoxia, whether or not the mother herself is symptomatic.
Why do some individuals develop SHS while others do not?
Two compensatory mechanisms prevent SHS in most patients:
- Carotid baroreceptors sense a decrease in blood pressure following a drop in venous return. In an attempt to restore cardiac output, they stimulate an increase in heart rate.
- Peripheral venoconstriction promotes venous return through the collateral vertebral and azygous venous systems that bypass the compressed IVC.
Collateral Venous Flow
Figure 1: Anatomy of the Collateral Venous System [4]
When the IVC becomes partially or fully obstructed, a well developed collateral system shunts blood from the iliac veins and deep venous plexus to the azygos system.
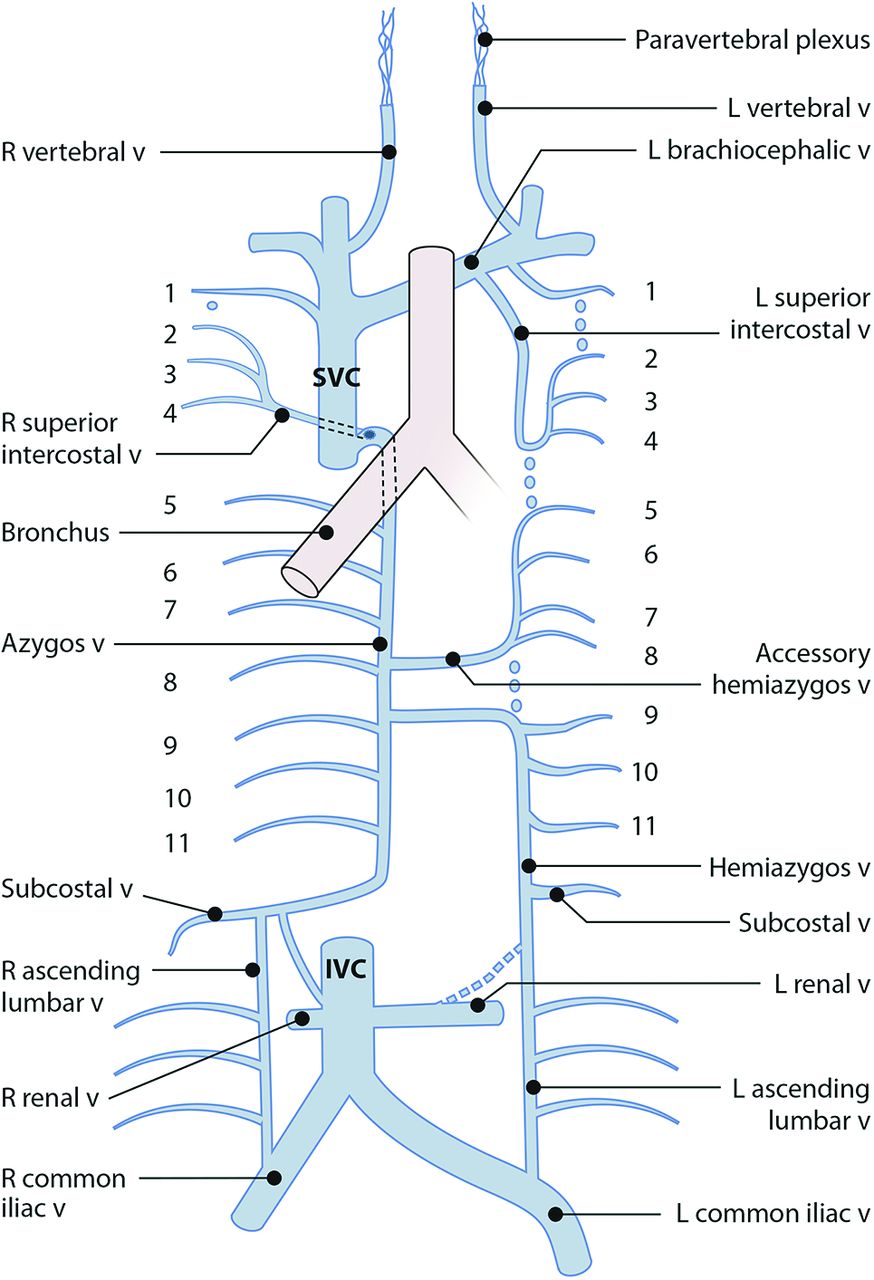
The azygos system is frequently dilated in pregnant women and provides an alternate pathway to the right atrium when the IVC is obstructed. The azygos vein on the right and hemiazygos vein on the left receive venous blood directly from the lumbar veins and rest of the deep collateral venous plexus.
Humphries et al [3] aimed to evaluate specific hemodynamic changes that occur in pregnant patients with SHS compared to those who do not develop the syndrome. They used MRI studies to measure blood flow through the aorta, IVC, SVC, and azygos vein, as well as hemodynamic parameters (cardiac output, heart rate and stroke volume). In their study, 12 patients without symptoms of SHS and 10 patients with self-reported SHS between 34-38 weeks’ gestation underwent MRI in the supine and left lateral positions.
In this very small study, both groups showed the following changes in the supine position compared to left lateral:
- Reduction in cardiac output, stroke volume and heart rate
- Reduction in blood flow through the IVC
- Increase in heart rate in the supine position
- Increase in blood flow through the azygos vein
Though both groups demonstrated increased blood flow through the azygos vein, symptomatic patients had a statistically significant reduction in azygos flow (L/min) compared to asymptomatic patients while maintaining a similar, and thus insufficient, increase in heart rate [1,3]. This study was limited by size, but it supports the theory that symptomatic patients have inadequate collateral compensation when caval flow is disrupted.

Figure 2: Difference in blood flow and hemodynamic parameters in patients with SHS and those without SHS in the supine position [3].
Special considerations on L&D
70-80% of American parturients receive neuraxial analgesia during labor [5], so clinicians must consider whether performing neuraxial will influence the severity of supine hypotensive syndrome. Patients who receive any form of neuraxial with local anesthetic will experience some degree of sympathetic blockade which blunts the peripheral vasoconstrictive response. In cases of a high neuraxial block (above T4), the spread of local anesthetic to the cardioaccelerator fibers may also impede the patient's ability to elevate her heart rate in response to a drop in cardiac output. In all patients with iatrogenic sympathectomy, there is the potential for maternal hypotension in the supine position to become exaggerated because of blunted compensatory mechanisms.
How can we prevent and treat supine hypotensive syndrome?
It is widely believed that SHS is a direct result of IVC compression by the gravid uterus with some contribution from aortic compression. How can we decompress these vessels and support cardiac output?
Left uterine displacement + adequate hydration +/- vasopressor support
A variety of non-standardized methods are used worldwide to try to achieve adequate left uterine displacement.
- Left uterine tilt (~15°)
- Wedge under the right pelvis (defined as upper gluteus maximus)
- Wedge under the lumbar spine (defined as above the iliac crest and below the lower costal region [6]
- Left lateral decubitus (90°)
- Manual left uterine displacement
How well does each method work?
Left lateral tilt was introduced to reduce the effects of aortocaval compression in the supine position when the full lateral position is not practical [7]. Left lateral tilt is achieved with a wedge under the right hip or right lumbar spine, or by tilting the entire bed (most feasible on an operating room table) to approximately 15 degrees. The recommendation for 15 degree lateral tilt was set arbitrarily in the 1970s, but until recently, had not been critically evaluated.
Pelvic wedge or lumbar wedge?
In 2008, Zhou et al [6] prospectively studied the impact of a lumbar wedge versus a pelvic wedge in hypotension during cesarean deliveries. They discovered that though both wedge positions resulted in substantial hypotension, the lumbar wedge was more effective than a pelvic wedge in reducing hypotension and vasopressor requirement after combined spinal-epidural anesthesia. Both groups had similar heart rate responses and neonatal APGAR scores and umbilical artery pH.
Degree of tilt?
Another small but interesting study of 10 pregnant and 10 non-pregnant patients by Higuchi et al [8] evaluated the effect of lateral tilt angle on the diameter and volume of the IVC and aorta as measured by MRI. In this study, women with obesity (body mass index > 30) and known supine hypotensive syndrome were excluded from recruitment. Higuchi et al demonstrated that we have been overestimating the benefit of left tilt on IVC compression as well as overselling the “aorto-” part of “aortocaval” syndrome.
Figures 3 & 4 (below) demonstrate the effect of left uterine tilt at 0°, 15°, 30° and 45° on the size of the IVC (hollow arrow) and aorta (solid arrow) in nonpregnant controls (A) and pregnant (B) patients. The size of the IVC changed slightly according to the position, while the abdominal aorta was not significantly different in any of the left lateral tilt positions.

Figure 3: IVC and aorta size in a nonpregnant control at different degrees of tilt

Figure 4: IVC and aorta size in a pregnant patients at term at different degrees of tilt
The hollow arrow identifies the IVC, which is completely compressed in term pregnancy in the supine and 15° positions, and only begins to fill at > 30° tilt. In contrast, the volume of the abdominal aorta was not significantly impacted by supine positioning or any of the left lateral tilt positions. There was also no difference in aortic volume between pregnant and nonpregnant patients in any position.

Figure 5: Mean volume of the aorta and IVC with 0°, 15°, 30° & 45° tilt in nonpregnant controls and term pregnant patients without symptoms of SHS
Higuchi et al's findings reinforce the theory that caval compression in the supine and low tilt angles is significant in pregnant patients at term. They also demonstrated that the aorta is more resistant to compression than previously assumed, thus challenging the prevailing theory that aortic compression has a significant contribution to SHS. This finding is supported by the landmark angiographic study from Bieniarz et al, that the aorta is typically laterally displaced in pregnancy, making it less vulnerable to compression [9].
In 2017, Lee et al [10] questioned the utility of 15° left lateral tilt in the setting of elective cesarean delivery and concluded after a prospective study of 108 patients undergoing elective cesarean delivery, that when optimal maternal and fetal conditions were maintained with fluid and phenylephrine, there was no apparent benefit to left lateral uterine displacement during cesarean delivery with respect to neonatal acid-base and clinical status [10].
Critics of the study argued that the phenylephrine requirements were higher (though still within a reasonable range) in the supine group versus the tilted group, and hemodynamic parameters such as cardiac output were also improved with the small degree of tilt. They argued that left lateral tilt for elective cesarean delivery should not be considered outdated dogma, and the relative low risk associated with tilting patients in the operating room means it should not be abandoned [11, 12].
Left lateral decubitus
Mendoca et al [13] demonstrated that the full left lateral position reduced the incidence of early hypotension compared with the tilted supine position (64 vs. 90%). They also described that patients tilted to 20° needed more support and tended to feel unsafe, some even asking to be returned to their supine position.
Manual Left Uterine Displacement
In cases of maternal cardiac arrest and resuscitation, the American Heart Association recommends manual left uterine displacement, or a left-lateral tilt of 27° to 30° if manual LUD is not possible [14]. Manual LUD is done by placing the provider's hand on the right side of the abdomen, lateral to the gravid uterus, and shifting the uterus to the left, off of the vena cava.

Let's Summarize:
Approximately ten percent of term pregnancies are complicated by supine hypotensive syndrome, due to IVC compression in patients with inadequate compensatory mechanisms.
There is strong evidence that left lateral tilt in the way it is routinely performed is generally ineffective at decreasing IVC compression and subsequent hypotension, though it may slightly reduce vasopressor requirement. A Cochrane analysis including an 857 cesarean deliveries reported no effect on SBP, incidence of hypotensive episodes, maternal heart rate, 5 minute APGAR scores or umbilical cord pH when comparing left lateral tilt to supine positioning [16]. It has also been demonstrated that manual left uterine displacement significantly increases cardiac output in patients who are already adequately tilted [17, 18].
How should we manage patients with SHS?
In the setting of labor, adequate maternal hydration in combination with left lateral decubitus positioning is often enough to prevent or treat SHS. In cases of fetal distress or severe maternal symptoms not relieved with basic interventions, vasopressors like phenylephrine or ephedrine may be used to temporize the situation.
Intravenous volume loading and vasopressor support are the mainstays of managing perioperative hypotension in both elective and non-elective cesarean delivery under neuraxial. We agree with Lee et al's response to criticism:
“ The goal of anesthetic management is not to maintain specific hemodynamic parameters, but rather to maintain adequate or optimal conditions for mother and fetus. Despite decades of practice and tradition, the evidence that the tilt maneuver, regardless of the degree at which it was provided, actually improves maternal or fetal conditions with contemporary neuraxial anesthesia practice is almost nonexistent [19]. ”
Supine Hypotensive Syndrome Key Points
- SHS develops in ~10% of term pregnancies due to inadequate compensation via the collateral venous system. Maternal compensatory mechanisms can be further compromised by neuraxial blockade.
- In cases of SHS, patients should be quickly positioned in left lateral decubitus and administered intravenous fluids. The head down position (Trendelenberg) can be used to immediately improve venous return in patients who are not actively vomiting.
- Combined spinal-epidurals are the preferred method for labor analgesia, as they allow for lateral positioning immediately following the procedure.
- Vasopressors should be considered in cases of extreme maternal hypotension (ie following spinal anesthesia), fetal decompensation, or in patients unresponsive to supportive maneuvers.
- Left lateral tilt is a low risk intervention, but 15° tilt is unlikely to influence maternal and fetal outcomes, especially when fluids and vasopressors are being administered.
- If you perform left lateral tilt, a lumbar wedge is superior to a pelvic wedge in reducing vasopressor requirement, and at least 30° tilt is needed to decompress the IVC
- Aortic compression has a minimal role in supine hypotensive syndrome, and as such, the term “aortocaval compression” probably should be revised.
1. Massoth, Christina; Chappell, Daniel; Kranke, Peter; Wenk, Manuel. Supine hypotensive syndrome of pregnancy: A review of current knowledge. European Journal of Anaesthesiology 39(3):p 236-243, March 2022. | DOI: 10.1097/EJA.0000000000001554
2. Howard BK, Goodson JH, Mengert WF. Supine hypotensive syndrome in late pregnancy. Obstet Gynecol 1953; 1:371–377
3. Humphries A, Stone P, Mirjalili SA. The collateral venous system in late pregnancy: A systematic review of the literature. Clin Anat. 2017 Nov;30(8):1087-1095. doi: 10.1002/ca.22959. Epub 2017 Aug 11. PMID: 28726308.
4. Borg N, Cutsforth-Gregory J, Oushy S, Huynh T, Savastano LE, Cloft HJ, Lanzino G, Brinjikji W. Anatomy of Spinal Venous Drainage for the Neurointerventionalist: From Puncture Site to Intervertebral Foramen. AJNR Am J Neuroradiol. 2022 Apr;43(4):517-525. doi: 10.3174/ajnr.A7409. Epub 2022 Jan 27. PMID: 35086801; PMCID: PMC8993202.
5. Butwick AJ, Bentley J, Wong CA, Snowden JM, Sun E, Guo N. United States State-Level Variation in the Use of Neuraxial Analgesia During Labor for Pregnant Women. JAMA Netw Open. 2018;1(8):e186567. doi:10.1001/jamanetworkopen.2018.6567
6. Zhou ZQ, Shao Q, Zeng Q, Song J, Yang JJ. Lumbar wedge versus pelvic wedge in preventing hypotension following combined spinal epidural anaesthesia for caesarean delivery. Anaesth Intensive Care. 2008 Nov;36(6):835-9. doi: 10.1177/0310057X0803600613. PMID: 19115653.
7. Crawford JS, Marilyn B, Davies P. Time and lateral tilt at caesarean section. Br J Anaesth 1972; 44:477–484.
8. Hideyuki Higuchi, Shunichi Takagi, Kan Zhang, Ikue Furui, Makoto Ozaki; Effect of Lateral Tilt Angle on the Volume of the Abdominal Aorta and Inferior Vena Cava in Pregnant and Nonpregnant Women Determined by Magnetic Resonance Imaging. Anesthesiology 2015; 122:286–293 doi: https://doi.org/10.1097/ALN.0000000000000553
9. Bieniarz J, Crottogini JJ, Curuchet E, et al. Aortocaval compression by the uterus in late human pregnancy II. An arteriographic study. Am J Obstet Gynecol1968; 100:203–217.
10. Allison J. Lee, Ruth Landau, James L. Mattingly, Margaret M. Meenan, Beatriz Corradini, Shuang Wang, Stephanie R. Goodman, Richard M. Smiley; Left Lateral Table Tilt for Elective Cesarean Delivery under Spinal Anesthesia Has No Effect on Neonatal Acid–Base Status: A Randomized Controlled Trial. Anesthesiology 2017; 127:241–249 doi: https://doi.org/10.1097/ALN.0000000000001737
11. Behnoosh Shayegan, Arjang Khorasani, Nebojsa Nick Knezevic; Left Lateral Table Tilt for Elective Cesarean Delivery under Spinal Anesthesia Should Not Be Abandoned. Anesthesiology 2018; 128:860–861 doi: https://doi.org/10.1097/ALN.0000000000002095
12. Riley ET, Dyer RA, Carvalho B: Left uterine tilt for cesarean delivery significantly improves maternal hemodynamics and should not be considered outdated dogma. Anesthesiology 2018; 128:858–9
13. Mendonca C, Griffiths J, Ateleanu B, Collis RE. Hypotension following combined spinal-epidural anaesthesia for Caesarean section. Left lateral position vs. tilted supine position. Anaesthesia 2003; 58:428-431.
14. Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, Jeejeebhoy FM, Gabrielli A: Part 12: Cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122(18 Suppl 3):S829–61
15. Zhang S. Figure 031_0788. Manual left uterine displacement by the 2-hand and 1-hand techniques. Illustration courtesy of Dr Shannon Zhang. - McMaster Textbook of Internal Medicine. empendium.com. Accessed September 28, 2023. https://empendium.com/mcmtextbook/image/B31.031_0788
16. Cluver C, Novikova N, Hofmeyr GJ, et al. Maternal position during caesarean section for preventing maternal and neonatal complications. Cochrane Database of Systematic Reviews 2013; CD007623.
17. Secher NJ, Arnsbo P, Heslet Andersen L, Thomsen A. Measurements of cardiac stroke Volume in various body positions in pregnancy and during Caesarean section: a comparison between thermodilution and impedance cardiography. Scandinavian Journal of Clinical and Laboratory Investigation 1979; 39: 569–76.
18. Kinsella SM. Lateral tilt for pregnant women: why 15 degrees? Anaesthesia. 2003 Sep;58(9):835-6. doi: 10.1046/j.1365-2044.2003.03397.x. PMID: 12911353.